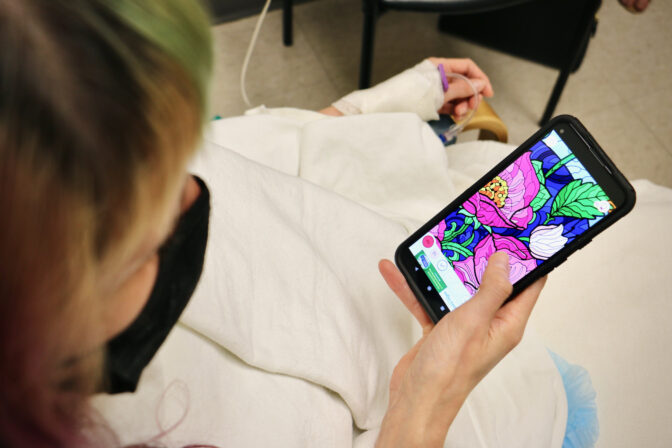
Lee Thompson sat in a pre-operative room, bundled in a blanket and socks, and played with an adult coloring book phone app to keep calm.
She had slept well the night before and refused to let herself feel anxious — even though she was about to undergo an elective surgery that would be difficult to reverse.
“I just don’t think it does me any good to be nervous,” Thompson said while waiting for medical staff to take her to the operating room. “So I’m just trying to stay relaxed and present.”
Emma Lee / WHYY
Lee Thompson passes the time with a coloring app as she waits in a room at Jefferson University Hospital to get a tubal ligation.
She never wanted to have kids. And at age 37, Thompson said she won’t ever change her mind. Over the years, the professional aerial acrobat from Philadelphia contemplated tubal sterilization (also known as tubal ligation) — a form of permanent birth control that involves either laparoscopic or open surgery to cut or remove the fallopian tubes.
When the U.S. Supreme Court overturned Roe v. Wade in June, Thompson’s decision became clear.
“I don’t want down the line to be stuck in any kind of really unfortunate position where I have to make really hard choices,” she said, noting that she wants freedom over her financial future.
“I entirely trust myself to make responsible decisions. And that includes the people that I choose to be with,” Thompson said. “What I don’t have control over is anything that could happen non-consensually. And I have very limited control over any decisions that the government may make around decisions I can make with my body.”

Emma Lee / WHYY
Lee Thompson waits in a room at Jefferson University Hospital, to get a tubal ligation.
Medical providers in states where abortion has already been outlawed — like Texas — have reported an uptick in requests for permanent birth control procedures following the Supreme Court’s Dobbs ruling. In Pennsylvania, abortion is still legal through 23 weeks of pregnancy, and later than 23 weeks if the pregnant person’s health is at risk. But uncertainty about the state of reproductive rights in the country — and a looming November election — has led some people in the Keystone State to make some serious considerations about how to permanently prevent pregnancy.
Luckily for Thompson, she faced no resistance when requesting to schedule the procedure with Dr. Rebecca Mercier, an obstetrician and gynecologist at Jefferson Health.
Mercier said that following the reversal of Roe, her office has received a spike in messages from concerned patients about contraception, as well as increased interest in tubal surgery.
She said her other patients have shared similar sentiments to Thompson.
“It’s something they’ve been considering and thinking about committing to,” said Mercier, who is also an assistant professor of family planning at Thomas Jefferson University. “And now, they really feel that they need to do everything that is available to them to prevent that unwanted pregnancy from happening to them in the future.”
And men, too, are opting for permanent birth control — Jefferson Health told WHYY News that primary care providers at the health system have seen an uptick in vasectomy interest following the overturn of Roe v. Wade. Jefferson referred 42 patients for vasectomies in July 2022. Before then, the monthly average for vasectomy referrals was 24.
According to the Centers for Disease Control and Prevention, 18% of women between ages 15 and 49 who use some form of contraception have undergone a sterilization procedure — making it the most common form of birth control in the country. That’s followed by birth control pills (14% of women in that age group), then intrauterine implants and devices (10%), then condoms (8%). Only around 5% use vasectomies as their main method to prevent pregnancy.
Dr. Laura Lindberg, a professor at the Rutgers School of Public Health who studies reproductive health, said she thinks there will be continued interest in permanent birth control procedures in a post-Roe world.
But, she emphasized that the Supreme Court decision has made procedures like tubal sterilization a “constrained choice.”
“I don’t think this is the perfect choice for everyone. It’s being made against other options being taken away,” Lindberg said. “We need to work to ensure that people have a full range of reproductive choices, including access to different types of contraception and abortion, to help them choose if or when to have a child. And sterilization is a valid and valuable choice, but shouldn’t be made because it’s the only choice that people feel that they have.”
If nothing else, physicians in the region say they hope the Roe decision will lead to more discussion and awareness about birth control methods, including tubal sterilization and vasectomy. And now, more than ever, physicians say it’s important to help their patients make informed decisions, while balancing their right to bodily autonomy.
Avoiding medical paternalism
Guidelines from the American College of Obstetricians and Gynecologists say physicians should respect their patients’ reproductive autonomy, while also counseling them about the permanence of tubal sterilization and explaining all of their birth control options.
However, there have been several anecdotal stories about younger, childless adults being denied tubal sterilization, according to experts interviewed for this story. The issue has prompted a Reddit page that lists physicians in each state who are “child-free friendly.”
One study, published in 2006 in the journal “Contraception,” found that people who have tubal sterilization under 30 are more likely to regret the decision than those over 30. Studies like this one might be one reason why some physicians have denied tubal sterilization to younger patients in the past, Mercier said.
These decisions should never be up to the provider, however, she and other physicians say.
Dr. Karen Antell, director of Maternity and Women’s Health Education at ChristianaCare, said she believes patient autonomy has improved over the years.
“Many more of our physicians, especially in OB-GYN, are female, and not educated in such a traditional environment where patients, especially female patients, were told what they should do,” she said.
Mercier said physicians must try to strike a balance between allowing personal autonomy and ensuring patients are fully aware that the procedure is permanent.
“It is not my responsibility, nor am I able to make sure that a patient won’t regret this decision in the future,” she said. “What my role is is to counsel the patients very clearly, be certain that they understand the permanent nature of the procedure, be certain that they understand … that there are people who do [regret it].”
Mercier said she has had patients who have regretted the procedure, but, “thankfully, that is a small number of patients.”
If a patient thinks there is a chance they might want to get pregnant in the future, other birth control methods are the better option, Antell said. But if a patient insists: “If that’s what she wants, then there’s no legal reason why we shouldn’t be providing that.”
Gloria Bachman, an OB-GYN and associate dean for women’s health at Rutgers Robert Wood Johnson Medical School, said it’s also important that the clinician make sure the patient is not making any decision under the influence of others.
“That decision to have a sterilization procedure should be done in an environment where there is no trauma, there’s no duress, there’s no one influencing that decision, including significant others that may be speaking for the women,” Bachman said. “Another point is the woman, or the trans man, should be counseled in a private setting without others around.”
Because of requirements in the Affordable Care Act, most health insurance companies cover the cost of tubal sterilization, but there are some disparities, Mercier said. Medicaid requires patients to wait 30 days between consultation and surgery. The requirement was put into place in the 1970s to protect patients, given the country’s history of non-consensual sterilizations.
Mercier said though the requirement might have good intentions, it means there’s an extra hurdle for Medicaid patients that commercially-insured patients don’t have to face.
“It is not something that stops most people, but it is an extra barrier, and the people who face that barrier are often our underserved, under-resourced communities,” she said.
That also means that people of color may be disproportionately lacking access to the procedure — in Pennsylvania, 42% of Black people and 43% of Hispanic people are on Medicaid, compared to 16% of white people.
Vasectomy: Like ‘having a cavity performed’
But the onus shouldn’t only fall on people who can get pregnant, Lindberg argues. Vasectomy in the U.S. is far less common than tubal sterilization and less common than it is in many other European countries — even though it’s a safer and less invasive procedure.
When the Affordable Care Act required contraceptive care — such as birth control pills, IUDs and sterilization procedures — to be covered by insurance, vasectomy was not included in the provision.
“There’s a bias in our country that protecting against pregnancy and contraception is a woman’s job and women’s responsibility,” Lindberg said, “and men are too often left off the hook or disengaged from that set of responsibilities and conversations around it.”
Josh Koplin, 45, recently got a vasectomy, a few months after his wife gave birth to their son, Theodore. They had decided they only wanted one child.
“Our kid is a great kid, but kids are hard,” said Koplin, an industrial designer and business owner who lives in Philadelphia.
The conversation Koplin had with his wife about vasectomy coincidentally happened around the same time that Roe was overturned. Though it wasn’t the cause of his vasectomy, the prospect of living in a post-Roe country amplified the decision, he said.
“I think it just made the whole thing feel a lot more real, and maybe more real than it needed to,” Koplin said. “It should have just been just a regular old decision, and it just put a big cloud over the whole thing.”
He admits that he was initially anxious about committing to the procedure.
“I did have a lot of those classic reservations that guys have, and it took me a month or so to wrap my head around it,” Koplin said, adding that his mind was eased after talking to friends who had undergone vasectomies.
Some research suggests that vasectomies might be less common than other methods of birth control because of misconceptions about sexual performance and masculinity. Several men who live in the Philadelphia region and have undergone vasectomies were unwilling to be interviewed for this story.
“Men do not talk about anything to begin with,” Koplin said. “When I talk to guys I know about this, there’s a reticence for them even to talk about it. They get very uncomfortable.”
People considering vasectomy should decide if it’s the right time in their life to end their ability to have kids, understanding that the procedure is permanent, said urologist Dr. Paul Chung, an associate professor at Thomas Jefferson University. A reversal requires a specialist, is not covered by insurance, and doesn’t guarantee success, he added.
Chung’s patients are of varied ages. They include: those who never want kids, who have kids and don’t want anymore, whose partner had challenging pregnancies, as well as patients with a genetic predisposition that they don’t want to pass on to their children.
“I don’t think that enough people are getting vasectomies. Hopefully people become more aware,” Chung said.
He also wants to clear up misconceptions about the procedure.
“It’s important for people to know that having a vasectomy done is not going to change erectile function. It’s not going to change hormones. It’s not going to change sexual performance. It’s not going to change how one urinates,” Chung said. “It’s not going to change anything in those types of ways.”
Most patients getting vasectomies receive local anesthesia to numb the area and are awake during the procedure. It can take as quickly as 10 minutes. Tubal sterilization, on the other hand, requires patients to be asleep, and the process takes about an hour.
“I really compare it to having a cavity performed. Obviously, nobody likes going to the dentist. Nobody likes to get the injection of pain medicine,” Chung said. “You can still kind of tell what’s being done, but you’re not in pain and you’re able to recover quickly without any pain medicine.”
Ultimately, Koplin said getting a vasectomy was the best decision for himself, and for his wife, who was previously using birth control pills.
“She has put up with a lot of sacrifice to carry and have our child. It’s not a fair equation, to put it mildly. And then that’s before we even talk about breastfeeding,” he said. “And I felt like, if there was one contribution I could make … I was like, ‘You know what? I could do this.’”
Post-sterilization: ‘I feel much more in control’
Thompson said her recovery has been easier and less painful than she thought it would be, and nine days after her surgery, she was able to practice aerials again. Thompson has since recorded some TikTok videos sharing her journey as an athletic person undergoing a medical procedure.
She said she expects scars to be practically unnoticeable — not that she cares, anyway.
“It’s so worth it. I’m just waiting for that tape to come off to see what it looks like. But if that’s just scars I have for sticking up for myself, then f**k yeah, you know?” Thompson said.
“Mostly I just felt so much less nervous, so much less anxiety and so much more freedom in the security that I have — like, ‘Hah hah, they can’t get me.’ Like the government can’t get me, like there isn’t a guy on this planet that can get me,” she said with a laugh. “I took the tracks off my baby train, and I’m so happy. I feel much more in control. I feel so much more relaxed.”




0 Commentaires